..
When you successfully complete your GP training, you will be issued with a Certificate of Completion of Training (CCT), which confirms you can work independently as a General Practitioner in the UK. To achieve CCT you need to satisfactorily complete the MRCGP assessment.
There are three components within the MRCGP that must be completed. Two of these are assessed externally - the Applied Knowledge Test (AKT) and the Recorded Consultation Assessment (RCA). The third is Work Place Based Assessment (WPBA), which is a set of structured tools used to assess your performance over time and captured in your e-Portfolio.
Below is some local information about satisfactory progression through your training, but for more detailed information please visit the RCGP website.
Please also see the following generic guidance regarding ARCP for all Scotland based trainees, please note there may be slight differences for GP trainees - ARCP Information.
This table (pdf) shows the capability and competence areas which underpin the RCGP training curriculum. To access the curriculum please follow this link to the RCGP website.
As mentioned above please find the attached E-portfolio Guidance for Satisfactory Progression at ARCP Panels (pdf), a COGPED and RCGP supported TeP guide created by the UK Deanery Assessment Reference Group.
A summary of this guidance, as well as the RCGP minimum requirements, is available in the next for download here (pdf)
OOH Training and requirements guidance
This ESR Checklist (pdf) may also be helpful for both trainees and trainers in preparation for planned reviews.
GPST3 ARCP REQUIREMENTS MANDATORY DOCUMENT ENSURE YOU COMPLETE AND UPLOAD THIS TO YOUR TeP FOR FINAL CCT ESR
Please also note the additional information below.
|
NOTE: OOH sessions |
If you have not completed your 108 hours in OOH before your ARCP is due (36 in ST1 and 72 in ST3) , your ES should document the dates of the remaining sessions and accumulated hours in your ESR. Under these circumstances missing OOH hours, if less than 6 hours, will not impact on ARCP outcome. However, if there is no documentation as to why OOH sessions are missing then an Outcome 5 missing evidence will be given
|
|
NOTE: SEA & AUDIT: Please also note the following from the RCGP:
|
Demonstration of competence in competency area 10 explicitly requires the trainee to provide evidence in the areas of SEA and audit. Although the need to write a structured report as per existing summative assessment requirements has been removed, the trainee will still need to demonstrate competence in these areas by participating in an audit and engaging in significant event processes. It will be up to the educational supervisor to assess competence in these areas through reviewing the evidence presented by the trainee at the regular reviews
|
|
NOTE: LEADERSHIP |
You will need to demonstrate evidence of leadership to meet the RCGP curriculum requirements e.g completing a LaMP course in ST3 or undertaking a QiP which demonstrates change management, chairing a meeting, engagement with Cluster work. There are other alternatives which may be suitable but which need to be clearly labelled and quality log entries |
|
NOTE: Fitness to Practice
|
There are 3 places that you should document sickness absence. · Fitness to Practice self-rating · Absence declaration as part of SOAR revalidation process (your regional administrators will email you) SOAR revalidation health statement (including all locum work, voluntary or paid work of any description
|
|
CCT Final documentation completion |
GPST3 ARCP REQUIREMENTS MANDATORY DOCUMENT ENSURE YOU COMPLETE AND UPLOAD THIS TO YOUR TeP FOR FINAL CCT ESR Please also note the additional information above. |
|
All e-portfolios are reviewed as part of the ARCP process to check the quality of the evidence provided by both you and your Educational Supervisor. FOR CCT you must have completed AKT and RCA in addition
|
|
GP trainees need to satisfy the GMC and the public that they have the appropriate knowledge, clinical skills and understanding of safeguarding and to be able to apply these skills when required. Safeguarding training is an integral and ongoing part of both GP training and professional development as a qualified GP. Please see documents below which details the requirements for Adult & Child Safeguarding in GP Training.
Adult and Child Safeguarding Requirements GP ST1 (PDF)
Adult and Child Safeguarding Requirements GP ST2 & ST3 (PDF)
Please see the RCGP website for further information
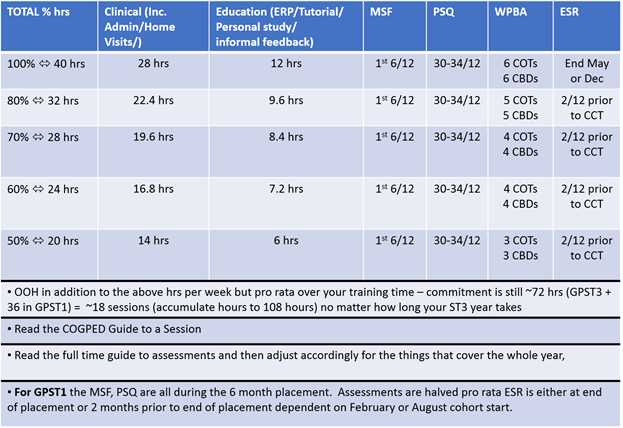
In summary LTFT WPBA arrangements are as follows:
Available for download is a year planner with suggestions to help you manage your training requirements. Please select the appropriate planner for the month that you first started your training.
Download the summary advice sheet here (pdf). Further information about reflective log entries is available at the AOMRC website
Try to see the potential of the EP as a resource to show your abilities, as a learning tool and keep the overall end in sight – showing progression can be satisfying and give a sense of achievement (plus preparing for appraisal and revalidation skills!). It is mandatory but don’t over think.
|
SUMMARY
|
Aim for quality log entries:
Targeted focussed entries:
Transferable skills make use of discussions you have had in assessments (CBDs and COTs) to focus the mind
The time factor – finding the time:
Ways of prompting yourself to do entries:
PDP - When considering your learning needs and how you will address these consider SMART:
Also consider the resources available to you to complete learning needs
Try to establish a dialogue with your supervisors:
This advice is available for download here (pdf).
The aim of the self-ratings is to self-assess your progress against the RCGP competency word pictures (see RGCP website). In doing this you can guide your educational supervisor to the robust evidence that you have gathered in your portfolio.
What makes good and effective self-ratings
|
Communication and Consultation Skills I have discussed complex patient problems requiring acute and long term care in my CBDs (see 12/11/15; 23/11/15 and also LLE 23/10/15; 25/09/15. I have developed my skills in using ICE in multiple settings see COT 21/10/15; 24/11/15 and LLE 11/09/15; 14/10/15. I have made some progress in dealing with patients whose agenda is different to mine see COT 22/09/15 and LLE 13/09/15 but I realise that I still struggle with this. I have attended a negotiating skills and dealing with difficult conversations course 21/08/15 in an effort to gain further skills. I have now applied that knowledge when dealing with a difficult and angry patient (LLE 21/10/15 and 26/11/15) |
You do this by
Pitfalls to avoid
The Applied Knowledge Test (AKT) is a summative test, which can be taken from ST2 onwards. It is computer-based and delivered at 150 Pearson VUE professional testing centres (driving test centres) around the UK. There are usually three sittings each year. For information about applying for and sitting the test, please follow this link to the RCGP website.
The Recorded Consultation Assessment (RCA) focuses on testing the areas of the GP curriculum (2018). The majority of trainees sit this examination in their ST3 year. Please check the Educational Opportunities page to see what resources your region can offer you to prepare for this. Full information is available on the RCGP website.
TIP: The more consultation practice you do in your normal working day i.e. seeing patients - the better prepared you are for passing RCA. Video your consultations and use for tutorials, do joint surgeries and get feedback from your educational supervisors.