Quality Improvement
As you may be aware, participation in Quality Improvement activity is a GMC requirement for revalidation, as well as being an NHS service requirement for those in Dental Practice. This page has been made available to inspire and assist SAS doctors and dentists in developing their own Quality Improvement projects, including ideas and example projects.
Benefits of Quality Improvement
For patients:
- Improve patient care by improving the quality and safety of care, access to care, patient experience
For the NHS:
- Improve quality and efficiency of care
- Potentially save money by improving service
For the SAS doctor/dentist:
- Develop skills in leadership
- Work as part of a successful team
- Improve care for your patients which could in turn improve job satisfaction
- Posters/presentations
- Looks good on the CV
Choosing a project
Start small and simple – use a PDSA cycle to guide you (more of that later)
Choose a common procedure – faster data collection, quicker results
A problem that affects you, your patients and your team (more likely to have cooperation from colleagues if they can easily see the value)
Something that matters to you (you will be more motivated to continue with it)
How to start
- Agree an aim – what are you focusing on and what do you want to change
- Clear change method – make sure that everyone understands the methods to be used
- Measure - how will you know that a change will be an improvement?
- Plan how to carry out the project – who will do what and when
- Plan for data collection – make sure that EVERYONE involved knows how and when to do this
- Think about how you will share your results – local meetings/posters/team meetings/publications?
Connect with your local QI department
Most hospitals will have their own QI department. They will usually help you to create forms/analyse date/refine your idea. Contact them at the outset – it could save you a lot of time and effort!
Ideas & themes for projects
- Reduce waste/avoid harm/improve consistency
- Improve patient safety or experience
- Assess outcomes against agreed standard and look for improvement measures
- Compliance with guidelines e.g IRMER
Examples of Completed Projects
1.) Audit of appropriate use of outpatient department appointments for routine biopsy results
Aims
- To avoid all unnecessary review appointments following routine biopsy investigations
Objectives
- To determine how many patients were discharged following biopsy
- To determine how many unnecessary return review appointments were booked
- To investigate the potential for a telephone review clinic
Method
A retrospective audit examining outpatient clinics cancelled due to COVID-19 was carried out. The total number of appointments was recorded for each clinic. Patient’s notes were examined to determine their outcome following telephone biopsy results. The number of discharged patients was recorded for each clinic
Results
- 28% of scheduled return routine appointments were not required
- 15% of all scheduled appointments not required
Recommendation
The introduction of a Core Trainee led telephone follow-up clinic to delivery biopsy results for patients to be discharged.
2.) The Introduction of the WHO Surgical Safety Checklist to Outpatient Sedation in an Outpatient Surgery Unit, An Improvement Project.
Aims
To ensure 100% compliance with the modified WHO Surgical Safety Checklist in operating lists in the outpatient department (OD)
- Modified paperwork and documentation to include modified checklist
- Brief and debrief templates
- Staff engagement, education and training
Outcome or Action Plan
A working group was created with representation from the whole team. Quality Improvement (QI) methodology was utilised and the WHO checklist was reviewed, tested and modified for suitability. An introductory session was held and included staff training. The percentage of lists using the modified checklist in the OD was measured. Only lists where the checklist was used for all patients are recorded as positive. Run charts were used to display improvements to the hospital. As per the NPSA and the SDCEP sedation guidance document, a log of adverse events, outcomes or never events was instated.
3.) OMFS Out of Hours Emergency Pathway
J Sweeney1, K Shekar2, N McGrath3
Oral and Maxillofacial Surgery
Ninewells Hospital
COVID19 has been an unprecedented situation which has changed our daily lives both at home and at work. When the lockdown commenced, Ninewells created a hospital within the hospital to safely manage COVID19. The entire set up of the hospital changed quickly, including our wards. A protocol was created for out of hours emergency patients requiring oral and maxillofacial surgery input. This focused on reducing patient footfall in the hospital and both patient and staff safety. OMFS in Ninewells covers Perth Royal Infirmary and Stracathro hospitals. There are multiple other referral pathways to our service including GPs, GDPs and other specialties within the hospital. All needed to be considered and included.
Aims
To establish a safe and effective pathway for out of hours emergency patients
Objectives
To create an official guidance document detailing the out of hours pathway
The original pathway was created on 28/3/20 and was split in to two clear sections:
- COVID positive/suspected COVID-positive patients - this section took into account the appropriate triage questions and route of entrance to Ninewells that patients must take.
- COVID-negative/Asymptomatic patients
All appropriate contact numbers and possible admission pathways were included in a flowchart to allow this to be easy to follow for all staff.
Where are we now?
Ninewells has further developed and now has three hospitals within the hospital. There is a red COVID-positive area, an amber indeterminate area and a green shielded pathway. The out-of-hours emergency pathway has been adjusted accordingly to reflect this and we are currently on our third version. Below is the correct pathway as of the 19/5/20 (Fig. 1.).
We have proven the ability to create a pathway at short notice and have learnt throughout this process. We continue to learn through this pandemic and will develop our pathway further as required.
Fig. 1. Current OMFS Out of Hours Emergency Pathway

4.) OMFS in the 21 Century – The development of virtual clinics
Sean Dolan
Oral and Maxillofacial Surgery
Ninewells Hospital, Dundee
Implementation of attend anywhere consultations within an OMFS department
Aims
- To reduce footfall within the Ninewells OMFS department during the COVID19 pandemic therefore reducing risk of transmission.
- Increase staff utilisation of the attend anywhere software.
Objectives
- To implement “Near Me” software into the Ninewells OMFS department.
- Train staff on use of attend anywhere software.
- Reduce number of in person appointments by having more ‘Near Me’ appointments.
Methods
As one of the current dental core trainees in the unit I was designated Near Me champion, this meant I was immediately involved in the set up and implementation of the service within the unit. In the first instance I had to decide who would require a Near Me account and when they would likely utilise this, in doing so I organised the user accounts for relevant members of staff. Webcams, headsets, and a new desktop were required, and I organised this along with their setup in the department. Following attendance at the online training, to streamline our department’s uptake, I trained the remaining individuals who would be utilising this service.
Results
Near Me was successfully implemented and all relevant clinicians received accounts to use the service. They were shown how to use it and then I assisted them with their first appointment so they could get used to its features. The appointment software we use “Trakcare” then had three clinics added to it for use during COVID19 – CVC in person, CVC telephone, and CVC Near Me. Patients were then divided amongst these clinics after appropriate triaging by various members of staff. There were three rooms available, initially we noticed a problem with the booking system as occasionally a Near Me would clash with a telephone call or in person appointment. However, we managed to rectify this and continued to see our patients effectively and in a timely manner.
There was a drastic increase in our number of Near Me appointments which one consultant was heavily involved in as these were being carried out from their home. Moving forward more staff intend to increase volume of Near Me appointments where possible.
The utilisation of the service was recorded for each department by the ‘Near Me’ team. Along with the survey results following each appointment of the patient’s opinions of the service. However, the former has been grouped together and is not collected for each clinician/department.
The service utilisation data has been organised in order of most to least used, the OMFS department is currently 10th with a total of 85 appointments (Fig1). Between April and May there was a roughly seven-fold increase in our departments number of appointments with the service. This increase may be attributed, in part, to the movement of many of the new referrals to one consultant who carried out these initial exams via Near Me.
Prior to COVID19 NHS Tayside was collecting its own data regarding patient satisfaction of the service; COVID19 has changed this, and the data collected is now done on a national level. Responses were overall positive, with most patients being very satisfied and willing to use the service again (71.1% and 97.9% respectively from Fig2).
The main issues it seems were to do with technical aspects, with 22% of people having such an issue. Sound quality appears to be an issue with 24.3% of those reporting a technical issue selecting this and 28.8% of those listing a disadvantage saying they could hear the other person properly (Fig2).
However, conversely, there were several benefits that patients agreed with, 21.8% of individuals felt it was safer/easier using this service due to their condition and 59.9% found it more convenient (Fig2). These figures cannot be ignored and show the overall positive response by patients.
Data was also collected regarding transport and mileage; I have excluded this from my report as I wanted to focus on the more technical aspects of the service. It is still wise to reflect upon this and therefore I have, with permission, reflected on some of this. Once again, in future, after the pandemic, it would be sensible for a future trainee to audit the patient satisfaction within the department.
|
Department |
March |
April |
May |
Total |
|
NHS Tayside CAMHS |
141 |
273 |
314 |
728 |
|
NHS Tayside Dermatology |
29 |
192 |
237 |
458 |
|
NHS Tayside Area Psychological Therapies |
5 |
105 |
313 |
423 |
|
NHS Tayside Physiotherapy |
0 |
200 |
201 |
401 |
|
NHS Tayside Adult Acquired Speech & Language |
23 |
67 |
199 |
289 |
|
NHS Tayside Child Health AHPs |
25 |
75 |
136 |
236 |
|
NHS Tayside Occupational Health |
0 |
77 |
138 |
215 |
|
NHS Tayside Respiratory |
3 |
105 |
93 |
201 |
|
NHS Tayside Mental Health Services |
0 |
36 |
57 |
93 |
|
NHS Tayside Oral & Maxillofacial |
0 |
9 |
76 |
85 |
|
NHS Tayside Palliative Medicine |
7 |
26 |
52 |
85 |
|
NHS Tayside Paediatrics |
0 |
18 |
62 |
80 |
|
NHS Tayside ENT |
0 |
32 |
45 |
77 |
Fig1; Abridged table from the Near Me monthly update in June recording the utilisation of Near Me consultations per service.
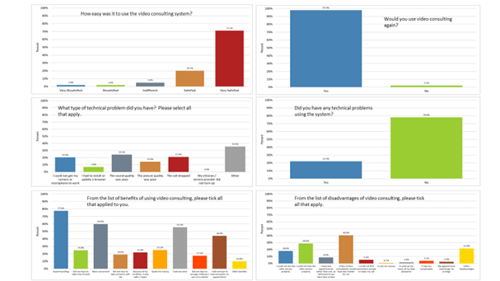
Fig 2; Patient survey responses for Near Me use. National data. Click here or on the image to enlarge
Discussion
Due to the COVID-19 outbreak it was determined that the OMFS unit in Ninewells hospital should utilise NHS Scotland’s “attend anywhere” service which uses Near Me software currently. This service was being rolled out by the Near Me team prior to COVID19 – however, this was not mandatory and therefore led to an inequity in access. It is used to let patients attend consultations from their own home using a smartphone or computer and internet connection. It aims to reduce footfall within the hospital especially during these trying times however, as noted earlier, it did exist before the outbreak. In turn, this can reduce spread of infectious diseases. Near Me has been approved for use by the Scottish government and is a secure form of video consultations. In future it would be very interesting to see the ongoing use of the service by various departments as part of their “new normal”
The first presentation of the virus in Ninewells was on the 2nd of March 2020. Our first ventilated case was the 10th March. Therefore, we worked on cancelling non-essential clinics and keeping our urgent cancer care only, however this left a cohort of patients who would ideally be seen but did not fit these criteria; this is where Near Me comes in.
There are two major drawbacks of the service we have noticed as a department. The first is that some patient groups do not have access to the necessary equipment to utilise the service. Secondly, even with the correct equipment we found it challenging to properly assess intra oral lesions which as a department we receive numerous referrals for.
Conclusion
Due to changing perceptions by patients it has been possible to implement a service such as Near Me, necessary even. Not only did we, as a hospital, decide to reduce the footfall, patients themselves were not always keen to attend if not required.
In the future it would be prudent to audit the patient satisfaction for our department only along with the user experience. This would allow changes to protocol within the department as well as aim to increase patient satisfaction where possible. The Dundee Dental Hospital may be implementing a similar service in its Restorative Department.
There will still be times where it is necessary to bring high-risk patients into the hospital and for new referrals of intra-oral lesions at the posterior limits of the oral cavity, a video call may not suffice. However, cases like that outlined above demonstrate why the implementation of this service was paramount during my time at the unit during the outbreak and why I am glad I was involved in managing this.
Acknowledgements
With thanks to the Near Me team for allowing use of the data they collected.
This page was last updated on: 30.09.2025 at 10.52